Why a MLH1/MSH2/MSH6/PMS2/EPCAM Somatic Tumor MMR Sequencing and Deletion/Duplication Test?
MMR Genes and Colon Cancer
Unlike other cells in the human body (for example the neurons in our brain that can live for decades), colon cells have a short lifespan of approximately 3-4 days. For this reason colon cells must replicate themselves at a constant rate. With each replication genetic mistakes are expected and normal. Fortunately, our DNA includes genes that act as repair tools that correct the mistakes made during cell replication. These are called Mismatch Repair (MMR) Genes.
MMR genes create a system for recognizing and repairing mistakes that arise during DNA replication. If the MMR genes themselves become damaged or mutated, they will not work properly and the mistakes made during replication will not be repaired. This leaves the cell vulnerable and unhealthy.
Cells without normal MMR genes can develop more and more mistakes with each new copy, resulting in a normal healthy cell losing the ability to stop dividing, or growing, once it has appropriately replaced itself. The ability to stop dividing, or growing, is what causes a colon cell to become cancerous.
Diagnosing MMR-related colon cancer
While only a small proportion of colorectal cancer (CRC) is caused by MMR gene damage, there is, a subset of CRC that can show signs that they could be caused by problems with the MMR repair process. The condition that is associated with MMR repair process deficiency is called Lynch syndrome.
Two of the most common tests that are performed on CRC tumor cells to determine if they are caused by MMR mistakes are immunohistochemistry (IHC) and microsatellite instability (MSI). Abnormal IHC or MSI results indicate that that there could be an underlying MMR abnormality contributing to the development of colon cancer cells.
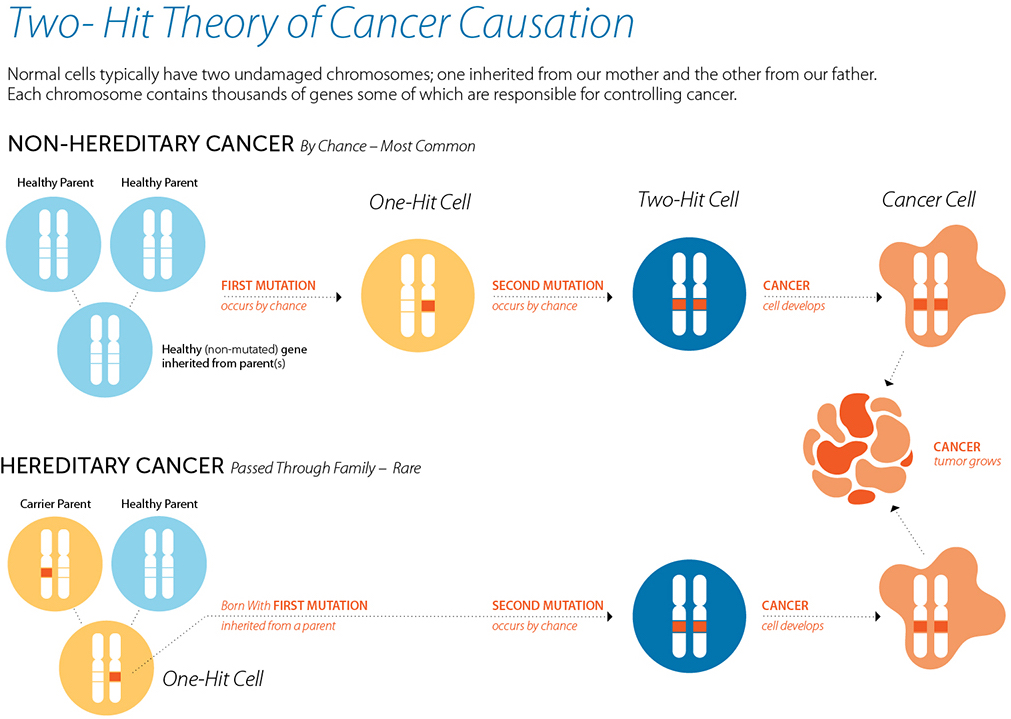
Heritable cancer and MMR
If a tumor cell shows signs of MMR deficiency (by IHC or MSI), the patient may be referred to speak with a genetic counselor. The genetic counselor will discuss that there are some people who are born with a mutated copy of one of their MMR genes and are, therefore, at a high risk for the development of colon cancer.
Patients with MMR deficiency and who meet criteria to be tested for hereditary cancer predisposition will have an option to be tested for Lynch syndrome. A blood sample may be studied to look for mutations in the genes MLH1, MSH2, MSH6, PMS2 and EPCAM.
People who have a positive test result, and are diagnosed with Lynch syndrome, have a significant increased risk of developing CRC. They also have an increased risk of developing other types of cancers, such as endometrial (uterine), stomach, breast, ovarian, small bowel (intestinal), pancreatic, prostate, urinary tract, liver, kidney, and bile duct cancers. Patients with Lynch syndrome have a 50% chance to pass the mutated gene, and associated cancer risk, to their children.
People who have a negative test result may have developed their cancer purely by chance as a result of two rare events in the single cell that developed into cancer. However, there is also a small possibility that the MMR gene mutation was not detectible in the blood sample, or that the cancer is related to MMR gene damage in just the cancerous cell. Answers to these questions may change the treatment the patient receives.
MMR abnormal tumors and normal Lynch (blood/germline) test results
CRC patients with normal MMR genes in their blood cells, or those without a hereditary predisposition to cancer, but who have MMR deficient tumors (by IHC or MSI), are sometimes referred to as having “Lynch-like” disease. While the tumor is shows MMR deficiency, the MMR genes in blood appear normal.
The National Comprehensive Cancer Network (NCCN) guidelines for Genetic/Familial High-Risk Assessment: Colorectal. Version 1.2022 suggest that in these cases the tumor should be checked for mutations in the genes MLH1, MSH2, MSH6, PMS2 and EPCAM.
If mutations are discovered in MMR genes in the tumor cells, our lab will go back and check again that neither of these mutations are present in the blood. By knowing where to look for mutations, it may be possible to identify mutations missed in previous testing. If the mutations are not found in blood, this result can help to rule out hereditary Lynch syndrome.
This unique category of patients that demonstrate MMR mutations in their tumor but not in their blood may be at increased risk for recurrent colon cancer compared to colon cancer that is not MMR deficient. Rodríguez-Soler, et al. 2013. Risk of Cancer in Cases of Suspected Lynch Syndrome Without Germline Mutation. Gastroenterology. 144:926–932.
Impact Genetics Somatic Tumor MMR Sequencing and Deletion/Duplication Test
This test is performed on samples of tumor/polyp tissue that were obtained at the time of initial surgery and are stored and saved in the pathology lab. A piece of this tissue is provided to our lab along with a fresh blood sample from the patient.
This test looks at genetic mutations in the tumor for the following genes; MLH1, MSH2, MSH6, PMS2 and EPCAM.
If mutations are discovered in these genes in the tumor cells, then the lab will look for these mutations in the blood sample to confirm whether the patient has Lynch syndrome or acquired somatic (tumor) mutations.

 Open-Expand Image
Open-Expand Image